CKD-KIDIGO

Evaluation and Management of Chronic Kidney Disease:Synopsis of the Kidney Disease:Improving Global Outcomes2012Clinical Practice Guideline
Paul E.Stevens,MBBS,BSc,and Adeera Levin,MD,BSc,for the Kidney Disease:Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members*
Description:The Kidney Disease:Improving Global Outcomes (KDIGO)organization developed clinical practice guidelines in2012 to provide guidance on the evaluation,management,and treat-ment of chronic kidney disease(CKD)in adults and children who are not receiving renal replacement therapy.
Methods:The KDIGO CKD Guideline Development Work Group defined the scope of the guideline,gathered evidence,determined topics for systematic review,and graded the quality of evidence that had been summarized by an evidence review team.Searches of the English-language literature were conducted through Novem-ber2012.Final modification of the guidelines was informed by the KDIGO Board of Directors and a public review process involving registered stakeholders.
Recommendations:The full guideline included110recommenda-tions.This synopsis focuses on10key recommendations pertinent to definition,classification,monitoring,and management of CKD in adults.
Ann Intern Med.2013;158:https://www.wendangku.net/doc/139698219.html, For author affiliations,see end of text.
*For a list of the members of the KDIGO CKD Guideline Development Work Group,see the Appendix(available at https://www.wendangku.net/doc/139698219.html,).
A decade of research after the publication of the?rst
internationally accepted de?nition and classi?cation of CKD(1)led the Kidney Disease:Improving Global Outcomes(KDIGO)organization to develop an updated Clinical Practice Guideline for the Evaluation and Man-agement of Chronic Kidney Disease(2).The updated guideline applied to all persons with chronic kidney disease (CKD)who were not receiving renal replacement therapy and included aspects related to both adults and children. Within the guideline,implications for clinical practice, public policy,and international considerations were high-lighted,along with areas of controversy,confusion,or non-consensus.The detailed work-up for speci?c causes of CKD was beyond the scope of the guideline,as were spe-ci?c approaches to acute kidney injury(AKI)and other acute kidney diseases,diagnostic work-up or treatment of speci?c causes of CKD,management of CKD in preg-nancy,detailed management of endocrine and metabolic complications,and detailed drug dosing.
The guideline sought to provide comprehensive guid-ance encompassing the whole CKD pathway,from early identi?cation and diagnosis through initiation of renal re-placement therapy for end-stage renal disease or end-of-life care.The recognition of the importance of patient safety and inclusion of caveats in the use and interpretation of commonly used tests was unique and highly practical. These details can be found in the full guideline(2),and recommendations are listed in the Supplement(available at https://www.wendangku.net/doc/139698219.html,).This synopsis focuses on the evalua-tion and classi?cation of CKD,areas that have generated substantial controversy.We also discuss some key recom-mendations,including the management of CKD progres-sion and complications,and the relationship between AKI and CKD.G UIDELINE D EVELOPMENT P ROCESS,E VIDENCE
G RADING,AND S TAKEHOLDER AND P UBLIC
C ONSULTATION
The work group consisted of an international group of clinicians and researchers,including kidney specialists, primary care physicians,a diabetologist,an epidemiologist, a clinical chemist,administrators,and a professional evi-dence review team.The work group formulated the scope of the guideline,graded evidence on the basis of the GRADE(Grading of Recommendations Assessment,De-velopment and Evaluation)system(3–5)(Appendix Ta-bles1and2,available at https://www.wendangku.net/doc/139698219.html,),and made con-sensus recommendations even when the quality of evidence was low to highlight key concepts and areas of confusion in clinical practice.In addition,the evidence review team did systematic reviews for8topics of interest(Appendix Table 3,available at https://www.wendangku.net/doc/139698219.html,),and searches were last con-ducted in June2011and supplemented with additional evidence through November2012.Further guideline de-velopment,evidence synthesis,and writing of the guideline itself was done by the work group.Full details of the guide-line development process,topic discussion,and consensus development can be found in the published guideline(2).
The draft guideline was reviewed by the KDIGO Board of Directors,and revisions were incorporated before a structured,Internet-based public review process.Feed-See also:
Web-Only
CME quiz
Supplement
Annals of Internal Medicine Clinical Guideline
back from this was reviewed by the work group,and?nal revisions were incorporated before publication of the guideline.
R ECOMMENDATIONS R ELATING TO THE D EFINITION AND
C LASSIFICATION OF CKD
1.1.1.CKD is de?ned as abnormalities of kidney struc-
ture or function,present for?3months,with implica-
tions for health.(Not Graded)
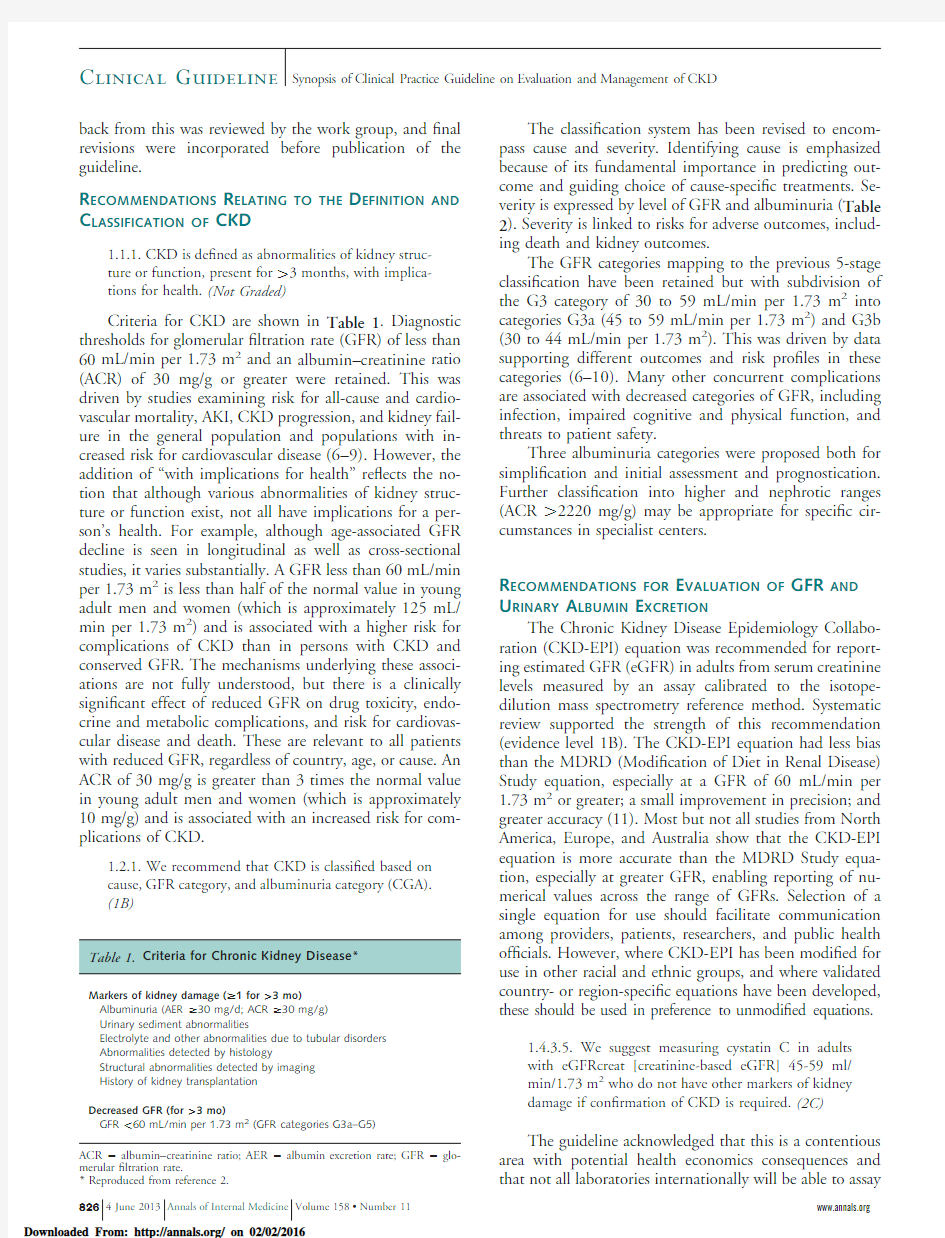
Criteria for CKD are shown in Table1.Diagnostic thresholds for glomerular?ltration rate(GFR)of less than 60mL/min per1.73m2and an albumin–creatinine ratio (ACR)of30mg/g or greater were retained.This was driven by studies examining risk for all-cause and cardio-vascular mortality,AKI,CKD progression,and kidney fail-ure in the general population and populations with in-creased risk for cardiovascular disease(6–9).However,the addition of“with implications for health”re?ects the no-tion that although various abnormalities of kidney struc-ture or function exist,not all have implications for a per-son’s health.For example,although age-associated GFR decline is seen in longitudinal as well as cross-sectional studies,it varies substantially.A GFR less than60mL/min per1.73m2is less than half of the normal value in young adult men and women(which is approximately125mL/ min per1.73m2)and is associated with a higher risk for complications of CKD than in persons with CKD and conserved GFR.The mechanisms underlying these associ-ations are not fully understood,but there is a clinically signi?cant effect of reduced GFR on drug toxicity,endo-crine and metabolic complications,and risk for cardiovas-cular disease and death.These are relevant to all patients with reduced GFR,regardless of country,age,or cause.An ACR of30mg/g is greater than3times the normal value in young adult men and women(which is approximately 10mg/g)and is associated with an increased risk for com-plications of CKD.
1.2.1.We recommend that CKD is classi?ed based on
cause,GFR category,and albuminuria category(CGA).
(1B)
The classi?cation system has been revised to encom-pass cause and severity.Identifying cause is emphasized because of its fundamental importance in predicting out-come and guiding choice of cause-speci?c treatments.Se-verity is expressed by level of GFR and albuminuria(Table 2).Severity is linked to risks for adverse outcomes,includ-ing death and kidney outcomes.
The GFR categories mapping to the previous5-stage classi?cation have been retained but with subdivision of the G3category of30to59mL/min per1.73m2into categories G3a(45to59mL/min per1.73m2)and G3b (30to44mL/min per1.73m2).This was driven by data supporting different outcomes and risk pro?les in these categories(6–10).Many other concurrent complications are associated with decreased categories of GFR,including infection,impaired cognitive and physical function,and threats to patient safety.
Three albuminuria categories were proposed both for simpli?cation and initial assessment and prognostication. Further classi?cation into higher and nephrotic ranges (ACR?2220mg/g)may be appropriate for speci?c cir-cumstances in specialist centers.
R ECOMMENDATIONS FOR E VALUATION OF GFR AND
U RINARY A LBUMIN E XCRETION
The Chronic Kidney Disease Epidemiology Collabo-ration(CKD-EPI)equation was recommended for report-ing estimated GFR(eGFR)in adults from serum creatinine levels measured by an assay calibrated to the isotope-dilution mass spectrometry reference method.Systematic review supported the strength of this recommendation (evidence level1B).The CKD-EPI equation had less bias than the MDRD(Modi?cation of Diet in Renal Disease) Study equation,especially at a GFR of60mL/min per 1.73m2or greater;a small improvement in precision;and greater accuracy(11).Most but not all studies from North America,Europe,and Australia show that the CKD-EPI equation is more accurate than the MDRD Study equa-tion,especially at greater GFR,enabling reporting of nu-merical values across the range of GFRs.Selection of a single equation for use should facilitate communication among providers,patients,researchers,and public health of?cials.However,where CKD-EPI has been modi?ed for use in other racial and ethnic groups,and where validated country-or region-speci?c equations have been developed, these should be used in preference to unmodi?ed equations.
1.4.3.5.We suggest measuring cystatin C in adults
with eGFRcreat[creatinine-based eGFR]45-59ml/
min/1.73m2who do not have other markers of kidney
damage if con?rmation of CKD is required.(2C)
The guideline acknowledged that this is a contentious area with potential health economics consequences and that not all laboratories internationally will be able to assay
ACR?albumin–creatinine ratio;AER?albumin excretion rate;GFR?glo-
merular?ltration rate.
*Reproduced from reference2.
Clinical Guideline Synopsis of Clinical Practice Guideline on Evaluation and Management of CKD
cystatin C.Evidence supports the use of cystatin C–based eGFR (eGFRcys)in persons without albuminuria (cate-gory A1)or other markers of kidney damage,especially those with an eGFRcreat of 45to 59mL/min per 1.73m 2(category G3a)(12,13).This group represents 3.6%of the U.S.population and 41%of persons in the United States estimated to have CKD on the basis of eGFRcreat and urinary ACR alone.Because the diagnosis of CKD in these persons is an area of substantial controversy with potential implications from disease labeling,the potential utility of a con?rmatory marker is https://www.wendangku.net/doc/139698219.html,e of eGFRcys to con-?rm CKD in populations has shown that two thirds of persons with eGFRcreat less than 60mL/min per 1.73m 2have a diagnosis of CKD con?rmed by eGFRcys less than 60mL/min per 1.73m 2and had markedly elevated risks for death,cardiovascular disease,and end-stage renal dis-ease compared with those with eGFRcys greater than 60mL/min per 1.73m 2.
1.4.4.
2.We recommend that clinical laboratories re-port albumin:creatinine ratios (ACR)and protein:crea-tinine ratios (PCR)in untimed urine samples in addition to albumin concentration or proteinuria con-centrations rather than the concentrations alone.(1B)
Measurement of urinary ACR was recommended for evaluation of proteinuria in preference to urinary total pro-tein for many reasons.Albumin is the most important pro-tein lost in the urine in most cases of CKD.In population studies,urinary ACR accurately predicts kidney and car-diovascular risks (6–9,14–19).Reduction in ACR in in-tervention trials targeted at blood pressure (BP)reduction or renin–angiotensin blockade has shown bene?t for pro-gression of CKD.Urinary ACR has greater sensitivity for detecting low-grade but clinically important albuminuria and is more precise at low but diagnostically important concentrations (20).
1.4.4.
2.1.The term microalbuminuria should no lon-ger be used by laboratories.(Not Graded)
Although the signi?cance of the A2category of ACR (30to 300mg/g)has been understood in persons with diabetes for decades,use of this category to denote CKD,especially in those with higher GFRs,remains controver-sial.However,data demonstrate that,at any level of GFR,an ACR increase above normal is associated with increased risk for adverse outcomes and that this increased risk is a continuum (6–9).It was,therefore,suggested that the term “microalbuminuria”no longer be used.
R ECOMMENDATIONS
FOR
M ONITORING CKD
Persons with CKD should be assessed at least annu-ally.The exact frequency of GFR and ACR monitoring will depend on the severity of CKD (Figure )and the risk for and rate of progression.Factors associated with pro-gression include cause of CKD,level of GFR,level of al-buminuria,AKI,age,sex,race or ethnicity,elevated BP,hyperglycemia,dyslipidemia,smoking,obesity,history of cardiovascular disease,ongoing exposure to nephrotoxic agents,and others.
Small ?uctuations in GFR are common and do not necessarily indicate progression.An approach involving an assessment of change in eGFR category con?rmed by a minimal percentage of change in eGFR (25%or greater)was recommended to de?ne progression.The reasoning for this was that although longitudinal cohort studies examin-ing progression have assumed that progression is linear,this is often not the case.The greater the ?uctuation in kidney function,the higher the probability of nonlinear progression (21,22).A criterion requiring both a change in GFR category (that is,from category G2to G3a)and per-centage of change would ensure that small changes in GFR (from 61to 59mL/min per 1.73m 2,for example,which
ACR ?albumin–creatinine ratio;AER ?albumin excretion rate;GFR ?glomerular ?ltration rate.*Relative to young adult level.
?In the absence of evidence of kidney damage,neither GFR category G1nor G2ful?ll the criteria for chronic kidney disease.?Including the nephrotic syndrome (AER usually ?2200mg/d [ACR ?2220mg/g]).
Clinical Guideline
Synopsis of Clinical Practice Guideline on Evaluation and Management of CKD
represents a change in category but a minimal change in GFR)would not be misinterpreted to represent progres-sion.Preliminary studies have indicated that this approach identi?es those at increased risk(23–25).
Data were insuf?cient to inform recommendations de-?ning albuminuria progression,although increasing levels of albuminuria suggest progression and has been shown to be associated with increased risk for adverse outcomes.
M ANAGEMENT OF CKD
Detailed within the guideline were many management recommendations for prevention of CKD progression and management of speci?c complications of CKD(see Sup-plement).Key recommendations relating to BP control, proteinuria reduction,AKI,and cardiovascular disease are summarized.
3.1.4We recommend that both diabetic and non-
diabetic adults with CKD and urine albumin excretion
?30mg/24hours(or equivalent)whose of?ce BP is
consistently?140mm Hg systolic or?90mm Hg
diastolic be treated with BP-lowering drugs to maintain
a BP that is consistently?140mm Hg systolic and
?90mm Hg diastolic.(1B)
3.1.5We suggest that both diabetic and non-diabetic
adults with CKD and with urine albumin excretion of
?30mg/24hours(or equivalent)whose of?ce BP is
consistently?130mm Hg systolic or?80mm Hg
diastolic be treated with BP-lowering drugs to maintain
a BP that is consistently?130mm Hg systolic and
?80mm Hg diastolic.(2D)
3.1.7We recommend that an ARB[angiotensin-
receptor blocker]or ACE-I[angiotensin-converting en-
zyme inhibitor]be used in both diabetic and non-
diabetic adults with CKD and urine albumin excretion
?300mg/24hours(or equivalent).(1B)
Control of blood pressure and reduction of proteinuria are critical in preventing CKD progression.Studies have consistently shown that reduction of proteinuria using
This GFR and albuminuria grid re?ects the risk for progression by intensity of coloring.The numbers in the boxes are a guide to the frequency of monitoring(number of times per year).Reproduced from reference2.ACR?albumin–creatinine ratio;CKD?chronic kidney disease;GFR?glomerular?ltration rate.
Clinical Guideline Synopsis of Clinical Practice Guideline on Evaluation and Management of CKD
renin–angiotensin–aldosterone system(RAAS)interrup-tion slows progression of both diabetic and nondiabetic nephropathy.Lowering blood pressure also slows CKD progression,breaking a potentially vicious cycle associating hypertension and CKD.Evidence is insuf?cient to recom-mend combining an angiotensin-converting enzyme inhib-itor with angiotensin-receptor blockers to prevent CKD progression.In formulating statements about blood pres-sure control and RAAS interruption,the recommendations in the KDIGO guidance on blood pressure control in CKD were followed to maintain consistency(26).
Lifestyle interventions(reduced sodium intake to?2g per day,achieving a healthy body mass index of20to25 kg/m2,smoking cessation,and exercising for30minutes5 times per week)and good diabetes control(target hemo-globin A1c level of7%)are also linked to reduction of proteinuria and alleviation of CKD progression(27–30).
3.1.12.We recommend that all people with CKD are
considered to be at increased risk of AKI.(1A)
The goal of this recommendation was to promote awareness of the complex relationship between CKD and AKI.Evidence demonstrates that CKD remains an inde-pendent risk factor for AKI,even after multivariate adjust-ment for comorbid conditions(31).Mounting evidence suggests that AKI is a risk factor for both incident CKD and progression of CKD.Both CKD and AKI increase in prevalence with age,and we are an aging population.
4.1.2We recommend that the level of care for ischemic
heart disease offered to people with CKD should not be
prejudiced by their CKD.(1A)
Persons with CKD are more likely to have a cardio-vascular event than to progress to end-stage renal disease; have worse prognosis with higher mortality rates after acute myocardial infarction;and higher risk for recurrent myo-cardial infarction,heart failure,and sudden cardiac death (32).Despite this,the level of care offered to persons with CKD is still frequently suboptimal.
D ISCUSSION
The CKD classi?cation system now encompasses cause of CKD,GFR category,and albuminuria category. This3-dimensional approach builds on the simpler earlier version,and the timing of these changes is appropriate, given the current familiarity of general physicians with the simpler version and the need to address common misun-derstandings in a systematic manner.It has been argued that additional factors,such as blood pressure,should be included within the classi?cation(33);however,while re-?ning the existing staging system,we also wanted to retain the simplicity and easy applicability of a classi?cation sys-tem in clinical,research,and public health practice.There-fore,we chose to include only kidney-related measures,and by including cause of CKD,we acknowledge the true dif-ferences in the natural history of kidney disease of different causes.The revised classi?cation provides a framework for the next decade of reporting and research in CKD.
Whether decreased GFR or increased ACR in older persons represents a disease or“normal aging”will always be debatable,and disease labeling will continue to provoke controversy in an aging society.Persons older than75years have a spectrum of GFRs exceeding60mL/min per 1.73m2with and without albuminuria,as well as values less than60mL/min per1.73m2.Aging is associated with accruing comorbid conditions and the use of medications that may result in reductions in GFR and albuminuria,and that is an underappreciated aspect of the argument about aging and eGFR.
It is no accident that37%of the recommendations in the guideline were ungraded and only10%were graded “A”for quality of the evidence.Much of the research gen-erated in the past decade has been aimed at de?nition and evaluation of CKD,together with identi?cation of persons with CKD and description of the associated adverse out-comes of CKD.We have some good trial data about inter-ventions,such as RAAS blockade in proteinuric CKD and use of statin therapy for CKD(34,35),and limited trial data in other areas,such as bicarbonate therapy for acido-sis.We need much more data if we want to affect out-comes.We need to know exactly which interventions are bene?cial in prevention or alleviation of both CKD pro-gression and the associated adverse outcomes and how and when these interventions should be applied.We also need to know when interventions that are believed to be bene-?cial may actually cause harm.For example,indiscriminate use of RAAS blockade in those with lower GFR and no speci?c indication other than hypertension may expose persons to additional risk for AKI with no bene?t.Allied to these areas,we need a much better understanding of de?-nitions of CKD progression and how they affect clinical practice and trials,how the relationship between AKI and CKD relates to progression,and whether we can positively in?uence this relationship.
From Kent Kidney Care Centre,East Kent Hospitals University NHS Foundation Trust,Canterbury,United Kingdom,and University of British Columbia,Vancouver,British Columbia,Canada.
Acknowledgment:The authors thank the KDIGO co-chairs Bertram L. Kasiske,Kai-Uwe Eckardt,David C.Wheeler;the evidence review team (Katrin Uhlig,Dana C.Miskulin,Amy Earley,Shana Haynes,Michael Cheung);and all those who provided feedback during the public review of the draft guideline.
Potential Conflicts of Interest:Dr.Levin:Consultancy(money to insti-tution):Abbott Laboratories,Merck&Co;Grants/grants pending(money to institution):Canadian Institutes of Health Research(CIHR),Kidney Foundation,Merck&Co,Ortho.Dr.Stevens:None disclosed.Disclo-sures can also be viewed at https://www.wendangku.net/doc/139698219.html,/authors/icmje/Con?ictOf InterestForms.do?msNum?M13-0034.
Clinical Guideline
Synopsis of Clinical Practice Guideline on Evaluation and Management of CKD
Requests for Single Reprints:Paul E.Stevens,MBBS,BSc,Kent Kid-ney Care Centre,Kent and Canterbury Hospital,Ethelbert Road,Can-terbury,Kent CT13NG,United Kingdom;e-mail,pstevens@https://www.wendangku.net/doc/139698219.html,. Current author addresses and author contributions are available at www https://www.wendangku.net/doc/139698219.html,.
References
1.National Kidney Foundation.K/DOQI clinical practice guidelines for chronic kidney disease:evaluation,classi?cation,and strati?cation.Am J Kidney Dis. 2002;39:S1-266.[PMID:11904577]
2.Kidney Disease:Improving Global Outcomes(KDIGO)CKD Work Group.KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease.Kidney Int Suppl.2013;3:1-150.
3.Atkins D,Best D,Briss PA,Eccles M,Falck-Ytter Y,Flottorp S,et al; GRADE Working Group.Grading quality of evidence and strength of recom-mendations.BMJ.2004;328:1490.[PMID:15205295]
4.Guyatt GH,Oxman AD,Kunz R,Falck-Ytter Y,Vist GE,Liberati A,et al; GRADE Working Group.Going from evidence to recommendations. BMJ.2008;336:1049-51.[PMID:18467413]
5.Uhlig K,Macleod A,Craig J,Lau J,Levey AS,Levin A,et al.Grading evidence and recommendations for clinical practice guidelines in nephrology.A position statement from Kidney Disease:Improving Global Outcomes (KDIGO).Kidney Int.2006;70:2058-65.[PMID:17003817]
6.Astor BC,Matsushita K,Gansevoort RT,van der Velde M,Woodward M, Levey AS,et al;Chronic Kidney Disease Prognosis Consortium.Lower esti-mated glomerular?ltration rate and higher albuminuria are associated with mor-tality and end-stage renal disease.A collaborative meta-analysis of kidney disease population cohorts.Kidney Int.2011;79:1331-40.[PMID:21289598]
7.Gansevoort RT,Matsushita K,van der Velde M,Astor BC,Woodward M, Levey AS,et al;Chronic Kidney Disease Prognosis Consortium.Lower esti-mated GFR and higher albuminuria are associated with adverse kidney outcomes.
A collaborative meta-analysis of general and high-risk population cohorts.Kidney Int.2011;80:93-104.[PMID:21289597]
8.Matsushita K,van der Velde M,Astor BC,Woodward M,Levey AS,de Jong PE,et al;Chronic Kidney Disease Prognosis Consortium.Association of esti-mated glomerular?ltration rate and albuminuria with all-cause and cardiovascu-lar mortality in general population cohorts:a collaborative https://www.wendangku.net/doc/139698219.html,ncet. 2010;375:2073-81.[PMID:20483451]
9.van der Velde M,Matsushita K,Coresh J,Astor BC,Woodward M,Levey A,et al;Chronic Kidney Disease Prognosis Consortium.Lower estimated glo-merular?ltration rate and higher albuminuria are associated with all-cause and cardiovascular mortality.A collaborative meta-analysis of high-risk population cohorts.Kidney Int.2011;79:1341-52.[PMID:21307840]
10.Levey AS,de Jong PE,Coresh J,El Nahas M,Astor BC,Matsushita K, et al.The de?nition,classi?cation,and prognosis of chronic kidney disease:a KDIGO Controversies Conference report.Kidney Int.2011;80:17-28.[PMID: 21150873]
11.Earley A,Miskulin D,Lamb EJ,Levey AS,Uhlig K.Estimating equations for glomerular?ltration rate in the era of creatinine standardization:a systematic review.Ann Intern Med.2012;156:785-95.[PMID:22312131]
12.Peralta CA,Shlipak MG,Judd S,Cushman M,McClellan W,Zakai NA, et al.Detection of chronic kidney disease with creatinine,cystatin C,and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality.JAMA.2011;305:1545-52.[PMID:21482744]
13.Waheed S,Matsushita K,Sang Y,Hoogeveen R,Ballantyne C,Coresh J, et https://www.wendangku.net/doc/139698219.html,bined association of albuminuria and cystatin C-based estimated GFR with mortality,coronary heart disease,and heart failure outcomes:the Athero-sclerosis Risk in Communities(ARIC)Study.Am J Kidney Dis.2012;60:207-16.[PMID:22537422]
14.Rifkin DE,Katz R,Chonchol M,Fried LF,Cao J,de Boer IH,et al. Albuminuria,impaired kidney function and cardiovascular outcomes or mortality in the elderly.Nephrol Dial Transplant.2010;25:1560-7.[PMID:20008829] 15.Gross JL,de Azevedo MJ,Silveiro SP,Canani LH,Caramori ML, Zelmanovitz T.Diabetic nephropathy:diagnosis,prevention,and treatment. Diabetes Care.2005;28:164-76.[PMID:15616252]16.Ninomiya T,Perkovic V,de Galan BE,Zoungas S,Pillai A,Jardine M, et al;ADVANCE Collaborative Group.Albuminuria and kidney function in-dependently predict cardiovascular and renal outcomes in diabetes.J Am Soc Nephrol.2009;20:1813-21.[PMID:19443635]
17.Viazzi F,Leoncini G,Conti N,Tomolillo C,Giachero G,Vercelli M,et al. Combined effect of albuminuria and estimated glomerular?ltration rate on car-diovascular events and all-cause mortality in uncomplicated hypertensive patients. J Hypertens.2010;28:848-55.[PMID:20087212]
18.Shastri S,Katz R,Shlipak MG,Kestenbaum B,Peralta CA,Kramer H, et al.Cystatin C and albuminuria as risk factors for development of CKD stage3: the Multi-Ethnic Study of Atherosclerosis(MESA).Am J Kidney Dis.2011;57: 832-40.[PMID:21296473]
19.Hallan SI,Ritz E,Lydersen S,Romundstad S,Kvenild K,Orth https://www.wendangku.net/doc/139698219.html,-bining GFR and albuminuria to classify CKD improves prediction of ESRD. J Am Soc Nephrol.2009;20:1069-77.[PMID:19357254]
https://www.wendangku.net/doc/139698219.html,mb EJ,MacKenzie F,Stevens PE.How should proteinuria be detected and measured?Ann Clin Biochem.2009;46:205-17.[PMID:19389884] 21.Li L,Astor BC,Lewis J,Hu B,Appel LJ,Lipkowitz MS,et al.Longitudinal progression trajectory of GFR among patients with CKD.Am J Kidney Dis. 2012;59:504-12.[PMID:22284441]
22.O’Hare AM,Batten A,Burrows NR,Pavkov ME,Taylor L,Gupta I,et al. Trajectories of kidney function decline in the2years before initiation of long-term dialysis.Am J Kidney Dis.2012;59:513-22.[PMID:22305760]
23.Turin TC,Coresh J,Tonelli M,Stevens PE,de Jong PE,Farmer CK,et al. One-year change in kidney function is associated with an increased mortality risk. Am J Nephrol.2012;36:41-9.[PMID:22699706]
24.Turin TC,Coresh J,Tonelli M,Stevens PE,de Jong PE,Farmer CK,et al. Short-term change in kidney function and risk of end-stage renal disease.Nephrol Dial Transplant.2012;27:3835-43.[PMID:22764191]
25.Turin TC,Coresh J,Tonelli M,Stevens PE,de Jong PE,Farmer CK,et al. Change in the estimated glomerular?ltration rate over time and risk of all-cause mortality.Kidney Int.2013.[PMID:23344477]
26.Kidney Disease:Improving Global Outcomes(KDIGO)BP Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease.Kidney Int Suppl.2012;2:337-414.
27.Jones-Burton C,Mishra SI,Fink JC,Brown J,Gossa W,Bakris GL,et al. An in-depth review of the evidence linking dietary salt intake and progression of chronic kidney disease.Am J Nephrol.2006;26:268-75.[PMID:16763384] 28.Navaneethan SD,Yehnert H,Moustarah F,Schreiber MJ,Schauer PR, Beddhu S.Weight loss interventions in chronic kidney disease:a systematic review and meta-analysis.Clin J Am Soc Nephrol.2009;4:1565-74.[PMID: 19808241]
29.Wakasugi M,Kazama JJ,Yamamoto S,Kawamura K,Narita I.A combi-nation of healthy lifestyle factors is associated with a decreased incidence of chronic kidney disease:a population-based cohort study.Hypertens Res.2012. [PMID:23171953]
30.National Kidney Foundation.KDOQI Clinical Practice Guideline for Dia-betes and CKD:2012Update.Am J Kidney Dis.2012;60:850-86.[PMID: 23067652]
31.Bedford M,Farmer C,Levin A,Ali T,Stevens P.Acute kidney injury and CKD:chicken or egg?[Editorial].Am J Kidney Dis.2012;59:485-91.[PMID: 22444492]
32.Herzog CA,Asinger RW,Berger AK,Charytan DM,D?′ez J,Hart RG, et al.Cardiovascular disease in chronic kidney disease.A clinical update from Kidney Disease:Improving Global Outcomes(KDIGO).Kidney Int.2011;80: 572-86.[PMID:21750584]
33.Burgos-Calderon R,Depine S.Systematic approach for the management of chronic kidney disease:moving beyond chronic kidney disease classi?cation.Curr Opin Nephrol Hypertens.2010;19:208-13.[PMID:19779338]
34.Remuzzi G,Benigni A,Remuzzi A.Mechanisms of progression and regres-sion of renal lesions of chronic nephropathies and diabetes.J Clin Invest.2006; 116:288-96.[PMID:16453013]
35.Baigent C,Landray MJ,Reith C,Emberson J,Wheeler DC,Tomson C, et al;SHARP Investigators.The effects of lowering LDL cholesterol with sim-vastatin plus ezetimibe in patients with chronic kidney disease(Study of Heart and Renal Protection):a randomised placebo-controlled https://www.wendangku.net/doc/139698219.html,ncet.2011;377: 2181-92.[PMID:21663949]
Clinical Guideline Synopsis of Clinical Practice Guideline on Evaluation and Management of CKD
Current Author Addresses:Dr.Stevens:Kent Kidney Care Centre, Kent and Canterbury Hospital,Ethelbert Road,Canterbury,Kent CT1 3NG,United Kingdom.
Dr.Levin:St.Paul’s Hospital,Providence Wing,Room6010A,1160 Burrard Street,Vancouver,British Columbia V6Z1Y8,Canada. Author Contributions:Conception and design:A.Levin.
Analysis and interpretation of the data:A.Levin.
Drafting of the article:P.E.Stevens,A.Levin.
Critical revision for important intellectual content:P.E.Stevens, A.Levin.
Final approval of the article:P.E.Stevens,A.Levin.Administrative,technical,or logistic support:A.Levin.
Collection and assembly of data:A.Levin.
A PPENDIX:KDIGO CKD G UIDELINE D EVELOPMENT
W ORK G ROUP M EMBERS
Rudy W.Bilous,Josef Coresh,Angel L.M.de Francisco, Paul de Jong,Kathryn E.Grif?th,Brenda R.Hemmelgarn, Kunitoshi Iseki,Edmund https://www.wendangku.net/doc/139698219.html,mb,Andrew S.Levey,Miguel C. Riella,Michael G.Shlipak,Haiyan Wang,Colin T.White,and Christopher G.Winearls.
Grade Level*Implications
Patients Clinicians Policy
1(“We recommend”)Most persons in this situation would—and only
a small proportion would not—want the
recommended course of action.
Most patients should receive the recommended
course of action.
The recommendation can be evaluated as
a candidate for developing a policy or
performance measure.
2(“We suggest”)Most persons in this situation would—but
many would not—want the recommended
course of action.Different choices will be appropriate for different
patients.Each patient needs help to arrive at a
management decision consistent with his or
her values and preferences.
The recommendation is likely to require
substantial debate and involvement of
stakeholders before policy can be
determined.
CKD?chronic kidney disease;GRADE?Grading of Recommendations Assessment,Development,and Evaluation;KDIGO?Kidney Disease:Improving Global Outcomes. *The additional category“Not Graded”was typically used to provide guidance on the basis of common sense or where the topic does not allow adequate application of evidence.
CKD?chronic kidney disease;GRADE?Grading of Recommendations Assessment,Development,and Evaluation;KDIGO
?Kidney Disease:Improving Global Outcomes.
AKI?acute kidney injury;CKD?chronic kidney disease;DM?diabetes mellitus;GFR?glomerular?ltration rate;KTR?kidney transplant recipient;NFD?nephrogenic?brosing dermopathy;RRT?renal replacement therapy.
Annals of Internal Medicine
