organic causes of chronic diarrhea

Lactulose/Mannitol Test Has High Ef?cacy for Excluding Organic Causes of Chronic Diarrhea
Vincenza Di Leo,Renata D’Inca`,Natalia Diaz-Granado,Walter Fries,Carla Venturi,Anna D’Odorico, Diego Martines,and Giacomo C.Sturniolo
Department of Surgical and Gastroenterological Sciences,University of Padova,Padova,Italy;University of Toronto,Toronto,Ontario,Canada;and Department of Internal Medicine,University of Messina,Messina, Italy
OBJECTIVES:Diagnosis in chronic diarrhea in the absence of a distinctive clinical pattern is often challenging,as bio-
chemical tests prescribed at the?rst evaluation do not show
enough sensitivity and speci?city to tailor further investi-
gation.Intestinal permeability to sugars is an accurate test
for detecting intestinal damage.The aim of this study was to
evaluate the diagnostic value of the lactulose/mannitol
(L/M)test in patients with chronic diarrhea. METHODS:We conducted a prospective cohort study to evaluate the diagnostic value of the L/M test in chronic
diarrhea.The test was administered to261consecutive
patients presenting with three or more bowel movements
daily for at least3wk.Biochemical tests including complete
blood cell count,acute phase reactive proteins,serum albu-
min and iron,and stool cultures for bacteria,ova,and
parasites were assessed at the same time.Additional diag-
nostic investigations were directed by clinical features as
well as?rst-line test results.
RESULTS:Over3yr,120(46%)of our patients were found to have an organic cause for chronic diarrhea,whereas in
141(54%)a functional condition was diagnosed.Multivar-
iate logistic regression analysis revealed that the L/M test
and C-reactive protein were independent predictors for the
?nal diagnosis of organic cause of chronic diarrhea,with
odds ratios of1.5(95%CI?1.29–1.78)and5.2(95%CI ?1.90–14.12),respectively.The area under the receiver operating characteristic(ROC)curve of the adjusted model
was0.82,with positive predictive value of80.4%and neg-
ative predictive value of77.7%.
CONCLUSIONS:The L/M test is a powerful tool for workup in patients with chronic diarrhea.Introducing the L/M test as ?rst-level test effectively improves the selection of patients who need further evaluation.(Am J Gastroenterol2003;98: 2245–2252.?2003by Am.Coll.of Gastroenterology)
INTRODUCTION
Chronic diarrhea is a nonspeci?c symptom that is often dif?cult to classify.Despite the frequent association with functional disorders,it can be the expression of organic disease such as in?ammatory bowel disease(IBD),celiac disease,chronic pancreatitis,and neoplasm(1–3).Medical history and physical examination are essential in guiding diagnostic decisions.In the absence of characteristic clinical signs,“?rst-line”biochemical and stool tests are prescribed. These tests should be able to indicate the presence of an organic disease and possibly address additional,more inva-sive investigations.However,these tests are limited by poor speci?city and sensitivity.Consequently,although?nal di-agnosis is achieved in about90%of cases(4),patients often undergo unnecessary or inappropriate procedures. Intestinal permeability re?ects the integrity of the intes-tinal mucosal barrier,which restricts the passive permeation of luminal substances(5).It is possible to assess intestinal permeability in vivo by measuring the urinary excretion of hydrosoluble and not degradable probes given orally.The lactulose/mannitol(L/M)test uses a mixture of two nonme-tabolized sugars,minimizing the in?uence of variables such as gastric emptying,intestinal motility,and renal function, which affect both markers equally.Moreover,it is a non-toxic,noninvasive test and the laboratory procedure is sim-ple and inexpensive(6).
Altered intestinal permeability has been reported in var-ious intestinal conditions associated with diarrhea such as celiac disease(7),IBD(8),infectious gastroenteritis(9–11), and food intolerance or allergy(12,13).The L/M test is used in the diagnosis and follow-up of celiac(14–16)and Crohn’s disease(17,18).Therefore,it may have the poten-tial to identify cases of chronic diarrhea with organic causes and may have the additional advantage of identifying the subgroup of patients with small bowel disease.
We examined the validity of the L/M intestinal perme-ability test in discriminating between functional and organic conditions associated with chronic diarrhea.The primary aim of the study was to determine whether intestinal per-meability to sugars,as measured by the L/M test,can improve selection of patients requiring further investigation. For this reason we prospectively administered the L/M test together with some of the most commonly used?rst-level biochemical tests.
T HE A MERICAN J OURNAL OF G ASTROENTEROLOGY Vol.98,No.10,2003?2003by Am.Coll.of Gastroenterology ISSN0002-9270/03/$30.00 Published by Elsevier Inc.doi:10.1016/S0002-9270(03)00703-2
MATERIALS AND METHODS
Patients
All consecutive patients referred to our outpatient clinic in a tertiary care center for chronic diarrhea from March,1997, to March,2000,were included in this prospective cohort study.Chronic diarrhea was de?ned as three or more bowel movements daily for?3wk,with no macroscopic evidence of mucus or blood.Patients complaining of signi?cant ep-isodes of colicky abdominal pain or systemic symptoms were excluded from the study.Patients with recent use(?3 months)of laxatives,nonsteroidal anti-in?ammatory drugs, sorbitol,or antibiotic therapy were not included in the study. No tests were performed in the stool to con?rm the absence of laxative compounds or sorbitol.
Patients were followed until diagnosis and for a minimum of6months thereafter,with a mean follow-up of12months. Informed consent was obtained from each patient.
Study Protocol
At the baseline visit,we collected medical history and performed physical examinations on each subject.These were followed by the evaluation of biochemical tests con-sisting of complete blood cell count,determination of acute phase reactant proteins,erythrocyte sedimentation rate,C-reactive protein(CRP),serum albumin and iron,stool cul-tures and search for ova and parasites for3consecutive days,urine examination,and the L/M test.The workup was blind with respect to the L/M test results.Second-line bio-chemical tests included antigliadin IgA and IgG antibodies, antiendomysial antibodies,thyroid stimulating hormone and serum thyroxine levels,skin prick test,Paper Radio Immu-nosorbent test(PRIST),and Radio Allergosorbent test (RAST).Diagnostic procedures such as abdominal ultra-sound or CT scan,upper GI endoscopy with duodenal bi-opsy,colonoscopy,and ileoscopy,and barium enema and small bowel follow-through were performed according to clinical suspicions.Additional tests such as GI peptides and hydrogen breath tests for evaluating possible endocrine tu-mors,disaccharidase de?ciency or bacterial overgrowth were also carried out when appropriate.
Measurement of Intestinal Permeability
A solution containing10g of lactulose and5g of mannitol in35ml of water(1300mOsml/L)was administered to each patient after an overnight fast.Urine was collected over the next6h in plastic containers with1ml of chlorexidine,2% as preservative,to prevent bacterial degradation of sugars. Patients were allowed to drink only water during the test.A 10-ml urine sample was stored at?20°C until assayed.An L/M ratio of0.030was the upper limit of normal for a group of35healthy subjects evaluated in our laboratory during the same time period(mean?3SD).
Sugars were measured by previously described methods and expressed as a percentage of urinary excretion(19,20). Brie?y,lactulose assay is based on hydrolization by?-ga-lactosidase in fructose and galactose,and enzymatically assaying fructose by standard methods(Boeringer-Mann-heim,Monza,Italy).The intrassay and interassay variabil-ities were4%and5.5%,respectively.Mannitol assay is based on formaldehyde production after periodic acid oxi-dation.Periodic acid(0.5ml)is added to the urine sample(2 ml)and allowed to stand at room temperature for10min. Stannous chloride(0.125mol/L)is added and the tube shaken until a milky precipitate develops.The precipitate is dissolved in5ml of chromotropic reagent and vigorously shaken,and the tube is then placed in a boiling water bath for30min.After cooling,the sample is increased to25ml with distilled water and allowed to stabilize at25°C in a water bath.The absorbance is read at570nm.Two test tube samples containing2ml of distilled water are used as controls;these undergo the same process as the sample tubes and are measured at the same time.The intra-and interassay precision was2.6%and6.9%,respectively.
Statistical Analysis
The outcome diagnosis of type of chronic diarrhea was categorized either as organic or functional.We considered increased erythrocyte sedimentation rate,CRP,and abnor-mal serum albumin and iron to be values?20mm/h,6 mg/L,?35g/L,and11?mol/L,respectively.The univar-iate statistics between these potential diagnostic determi-nants and the presence of an underlying organic cause for chronic diarrhea were quanti?ed using?2statistics for cat-egorical variables and two-tailed t tests for numerical vari-ables.An association was considered to be statistically sig-ni?cant at p?0.05.A multivariate logistic regression model was constructed to evaluate the effect of each pre-dictor on chronic diarrhea diagnosis by including all param-eters with p?0.10from the univariate analyses.We began by constructing a logistic regression model that would con-tain the main predictors,using backward stepwise variable selection.The?nal model was then adjusted with confound-ers(gender,age)that were identi?ed a priori,thus obtaining our adjusted model.The reliability(goodness of?t)of each model was assessed using the Hosmer-Lemeshow test,and the discriminative power of the model was assessed using the area under the receiver operating characteristic(ROC) curve(21).The area under the ROC curve is an ideal measure to summarize the discriminative power of a diag-nostic model,with a value of1.0representing100sensitiv-ity and speci?city,and a value of0.5representing no dis-criminatory power.These models were used to generate ROC curves plotting the sensitivity against the false positive rate(or1–speci?city)at different cut-off points from0.001 to0.231.The distribution of probabilities for the diagnosis of organic chronic diarrhea is represented through the cut-off points,adjusted for age.
RESULTS
A total of274consecutive patients were eligible for our study.Mean duration of the symptom was24days(range
2246Di Leo et al.AJG–Vol.98,No.10,2003
21–31).Thirteen patients had a diagnosis of infectious/parasitic diarrhea and were excluded;therefore a total of 261patients were enrolled in the study.Patient characteristics are shown in Table 1.
Final diagnoses are listed in Table 2.A comparable num-ber of procedures were performed in the group of patients with organic disease and in the group with functional con-ditions (Table 1).
An organic cause of chronic diarrhea was found in 120cases (46%).A total of 39patients were diagnosed with
enteropathy.All 28patients with celiac disease had a char-acteristic histological pattern and high antigliadin antibodies titers before diet,which normalized after 6months of diet-ing.Crohn ’s disease involving the small bowel was diag-nosed in 10patients.PAS staining showed presence of Tropheryma whippleii in an ileal biopsy of the patient di-agnosed with Whipple ’s disease.Among the 52patients with colonic diseases,seven had ulcerative colitis and ?ve had colonic Crohn ’s disease.A total of 21patients had diverticula with no in ?ammation.In the 12patients with acute self-limited colitis,acute mucosal in ?ammation and nonspeci ?c histological features of ?ogosis were found.Microscopic colitis (four patients),ischemic colitis (two patients),and colon cancer (one patient)were the other colonic causes of chronic diarrhea.In the miscellaneous group (29patients),the eight diagnoses of food intolerance or allergy were based on either skin prick tests or serum IgE level,and responses to diet and breath test were used to detect the two cases of bacterial overgrowth.Five nonvil-lous polyps ?1cm in diameter were found in ?ve patients whose colonoscopies were otherwise normal.Hyperthyroid-ism (three patients),alcohol abuse (three patients),chronic pancreatitis (three patients),and diabetes (two patients)were also atypical causes of chronic diarrhea.Finally,none of the neoplasms (three patients)in this group involved the small bowel.
A total of 141subjects had a ?nal diagnosis of functional disorder on clinical diagnostic workup and long term fol-low-up.In all,120patients were classi ?ed as having IBS.Sixteen patients had ileal follicular hyperplasia documented by histology with no alteration of serum level of immuno-globulins.Other conditions associated leading to functional diarrhea were anal sphincter incontinence (two patients),psychiatric disorders (two patients),and postsurgical adhe-sions (one patient).
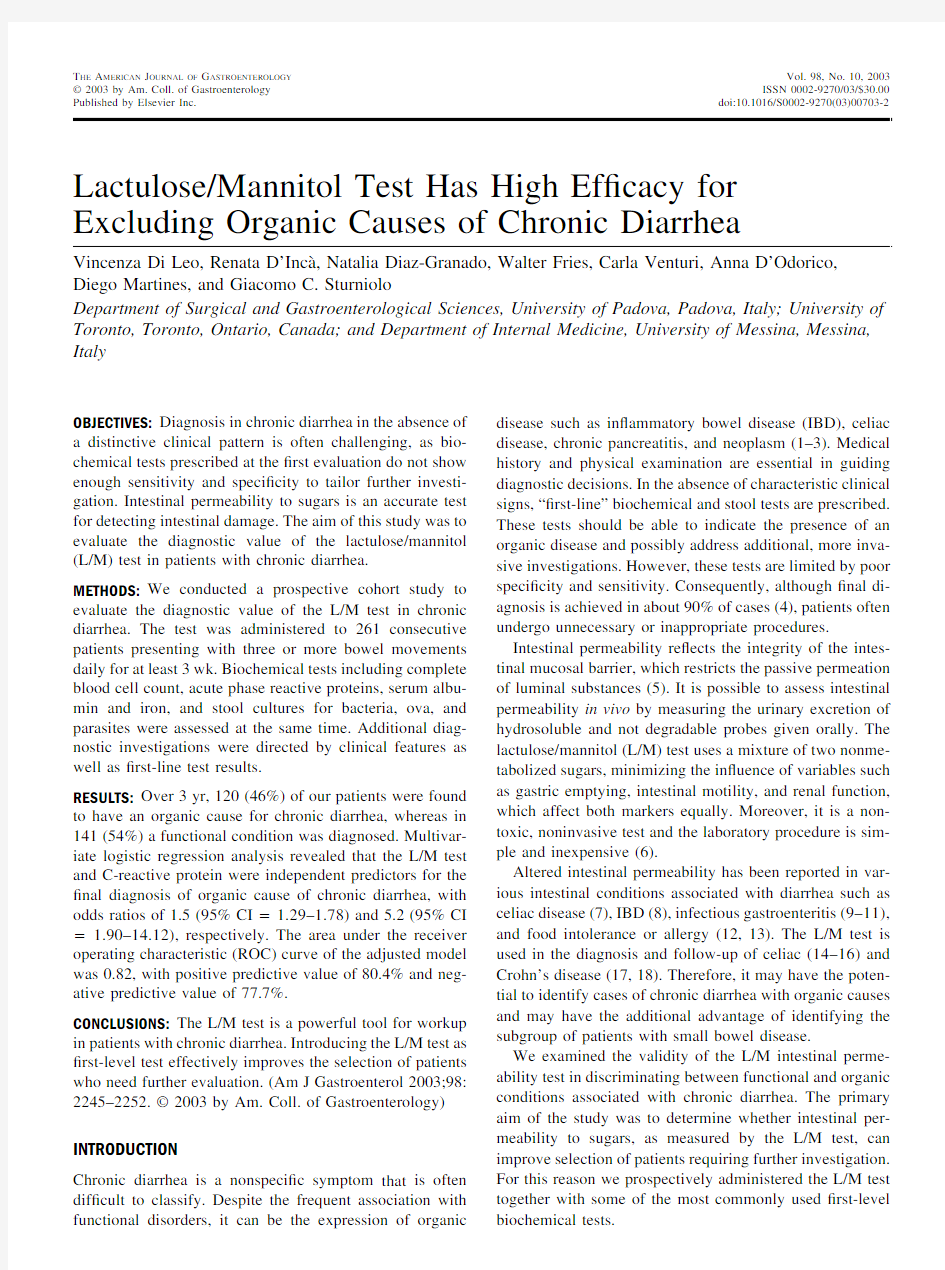
The presence of organic disease was signi ?cantly asso-ciated with L/M test results ?0.030(p ?0.0001)and with serum iron level ?11?mol/L (p ?0.001)(Table 3).The distribution of the altered L/M test with respect to the ?nal diagnosis is shown in Figure 1.The mean value of the L/M
Table 1.Baseline Characteristics of Participating Subjects
Characteristic All (n ?261)Organic (n ?120)Functional (n ?141)p Value*Age (yr)
Mean (SD)(range)37(15)(18–83)42(17)(18–83)34(12)(18–74)?0.001Sex
%M:F (n)39:61(102:159)34:66(39:76)43:57(63:83)ns Procedures %(n)
Endoscopy (upper GI)65(171)66(76)65(95)ns 68(178)67(77)69(101)ns Colonoscopy
Small bowel follow-through/barium enema 5(13)4(5)5(8)ns Abdominal US
38(99)
38(44)
38(55)
ns
*Comparisons were made between patients diagnosed with organic and functional causes for chronic diarrhea.
Table 2.Final Diagnoses Associated With Chronic Diarrhea
Underlying Cause No.of Patients
Organic diseases (n ?120)Small bowel (n ?39)Celiac disease 28Crohn ’s disease 10Whipple disease 1Colon (n ?52)
Diverticular disease 21ASLC
12Ulcerative colitis 7Crohn ’s disease 5Microscopic colitis 4Ischemic colitis 2Colon cancer
1Miscellaneous (n ?29)Food allergy 8Polyp
5Hyperthyroidism 3Alcohol abuse
3Chronic pancreatitis 3Bacterial overgrowth 2Diabetes
2Carcinoid (surrenal gland)
1Pancreatic cancer 1Oat cells carcinoma
1Functional diseases (n ?141)IBS
120Ileal follicular hyperplasia 16Incontinence
2Psychiatric disorder 2Postsurgical adhesion
1
ASLC ?acute self-limited colitis.
2247
AJG –October,2003Lactulose/Mannitol Test in Chronic Diarrhea
test in the group with organic disease was signi ?cantly increased compared to that in the group with functional conditions (0.043?0.0004vs 0.016?0.0001,respec-tively;p ?0.0001).Mean L/M values ?SE and range according to the ?nal diagnosis are shown in Table 4.The L/M test was abnormal in 52of 120patients with ?nal diagnosis of organic disease and in 13of 141patients with a functional condition.All patients with a ?nal diag-nosis of celiac disease had altered L/M test.Among the 21patients diagnosed with IBD,nine had increased intestinal permeability.Three patients with diverticula had also ab-normal L/M test results.The L/M test was also altered in two patients with chronic alcohol abuse and in three patients with food allergy.In the group of functional conditions,
seven patients with increased L/M test had ileal follicular hyperplasia.
The tests for CRP,serum iron,and L/M were selected for multivariate logistic regression.Only CRP and L/M were independent predictors for the diagnosis of chronic diarrhea with an underlying organic disease,with odds ratios of 5.2(95%CI ?1.90–14.12)and 1.5(95%CI ?1.29–1.78),respectively (Table 5).The area under the ROC curve was 0.59for the model with CRP alone,indicating a poor dis-crimination.Inclusion of L/M test in the model raised the area under the ROC curve to 0.76(Fig.2).Adjusting for age (gender was not a statistically signi ?cant confounder)re-sulted in a further increase in the area under the ROC curve to 0.82(Fig 3).(This indicates that in 82%of the cases,a randomly selected patient with an organic cause underlying chronic diarrhea will have increased L/M test and CRP level,and a randomly selected patient with chronic diarrhea caused by a functional condition will have L/M test and CRP level within the normal range.)The model had a positive predictive value of 80.4%and a negative predictive value of 77.7%.
Finally,by stratifying patients diagnosed with an organic disease in three groups (i.e.,small bowel diseases,colonic diseases and miscellaneous),the L/M test was able to iden-tify small bowel diseases with 90%sensitivity and 87%speci ?city at a cut-off point of 0.030.
Table 3.Percentage of Abnormal Biochemical Tests in Each Dis-ease Category
L/M
CRP Serum Iron Whole population 201216Functional disorders 955Organic diseases
452230Small bowel disease 873164Colonic disease 172322Miscellaneous 29
86p
?0.0001
0.087
?
0.001
Figure 1.Distribution of L/M values in patients with chronic diarrhea.
Table 4.Values of the L/M Test According to the Final Diagnosis
N
Mean ?SE (range)Functional disorders 1410.016?0.0001(0.001–0.135)Organic diseases
1200.043?0.0004(0.001–0.231)Small bowel diseases 390.086?0.013(0.011–0.231)Colonic diseases 520.021?0.0003(0.002–0.088)Miscellaneous
29
0.023?0.0008(0.001–0.068)
Table 5.Multivariate Logistic Regression to Predict the Presence of Organic Causes for 261Patients Presenting With Chronic Diarrhea
Explanatory Variable Odds Ratio (95%CI)p Value Model 1
Increased C-reactive protein* 6.77(2.67–17.16)?0.0001Model 2(?nal)
Increased C-reactive protein*
5.20(1.90–14.21)0.001L/M test per 0.01increase
1.51(1.29–1.78)?0.0001Model 3(adjusted)Increased C-reactive protein*
6.38(2.16–18.85)?0.001L/M test per 0.01increase 1.56(1.32–1.85)?0.0001Age per 10-yr increase
1.62(1.32–1.99)
?0.0001
*Increased C-reactive protein was considered to be ?6mg/L.
2248Di Leo et al .AJG –Vol.98,No.10,2003
DISCUSSION
The diagnostic algorithm for chronic diarrhea is not univer-sally applicable and standardized.Furthermore,it may in-clude unnecessary and invasive procedures,which could be more ef ?ciently used with a proper characterization of dis-ease of the patients.Although chronic diarrhea may be associated with organic diseases,the most common cause of this symptom in Western countries is a functional disorder (22).Therefore a simple,noninvasive,and inexpensive test that could help in deciding the workup would be welcomed by clinicians,patients,and health care administrators.
In this study,we prospectively evaluated the diagnostic value of measuring intestinal permeability to sugars as a ?rst-line test in a cohort of 261consecutive patients with chronic diarrhea of unknown etiology.Our results show that the L/M test can signi ?cantly identify the presence of or-ganic disease underlying chronic diarrhea.Among the other ?rst-line tests that we considered,only CRP was an inde-pendent predictor of organic causes of diarrhea.However,using the ROC analysis,we have shown that only the combination L/M test and CRP has a real discriminating capacity,being able to correctly classify chronic diarrhea into underlying organic or functional disease.
Intestinal permeability to sugars is a reliable marker for small bowel disease (23);however,there are few data con-cerning its diagnostic ability in other GI conditions.A previous study evaluating intestinal permeability to sugars in chronic diarrhea was conducted in a pediatric population,and showed a highly signi ?cant correlation between the test results and small bowel morphology (24).On the other hand,it has been reported that in acute ulcerative colitis Cr-EDTA excretion is increased (8)and the L/M test could be abnormal (25).During infectious colitis (11)and shigel-
losis (10),intestinal barrier function is perturbed.Increased permeation of intestinal epithelium has also been related to alcohol consumption (26)and food allergy (13,27).Our results show that even in a nonselected adult population the L/M test is a reliable marker for the presence of organic disease.
Most studies on diagnostic tests for chronic diarrhea have identi ?ed sensitive and speci ?c markers for colonic in ?ammation (28,29).Considering our exclusion criteria (presence of mucus and blood,colicky abdominal pain,and systemic symptoms),the most common cause of organic diarrhea in our population was located in the small bowel,in agreement with previous reports (22,30).In small bowel disease,diarrhea is mainly caused by malabsorption,even in the presence of in ?ammatory fea-tures (31).Among the 39patients with a ?nal diagnosis of small bowel disease,34had increased intestinal per-meability.Moreover,in seven of these patients,the L/M test was the only abnormal ?nding.In the work by Juby et al.(32),more than 1000children with symptoms suggestive of celiac disease were evaluated and the sen-sitivity of the L/M test for small bowel lesions was 94%(31),value corroborated in subsequent studies (15,23,33).Lower sensitivity was reported by Catassi et al.,in whose study 50%of the patients screened for celiac disease had normal intestinal permeability (34).How-ever,this study was performed using an isotonic solution of sugars,which has been shown to be less sensitive in detecting damage to small bowel mucosa (35)and which had a highly conservative cut-off.In our study,antien-domisial antibodies were positive in all but one patient with a ?nal diagnosis of celiac disease,whereas all of these patients had increased L/M test results.A recent study (36)showed that a single serological marker
may
Figure 3.Receiver operating characteristic curve for the CRP and L/M test adjusted by age (model 3).NPV ?negative predictive value;PPV ?positive predictive
value.
Figure 2.Receiver operating characteristic curve for the CRP level (model 1)and the CRP plus L/M test (model 2).CRP ?C-reactive protein;L/M ?lactulose/mannitol.2249
AJG –October,2003Lactulose/Mannitol Test in Chronic Diarrhea
be not suf?cient for diagnosing celiac disease in asymp-tomatic subjects.Considering the high prevalence of ce-liac disease,which is equivalent in Europe and the United States(37),the L/M test could represent a valid and cost-effective complementary tool in screening for this condition.
Compared to the more commonly tested acute phase reaction proteins,the L/M test was shown to be more spe-ci?c for detecting organic causes of chronic diarrhea in our population.However,considering the wide range of dis-eases diagnosed in our patients,its sensitivity was not sat-isfactory.Therefore,we performed a multivariate regression analysis,including all tests that were shown to be signi?-cantly associated with diagnosis of organic disease at the univariate statistic.To allow an unbiased selection of the best test or combination of tests for diagnosis,we purposely choose a conservative p value(?0.10).Our study revealed that increased CRP and increased L/M test,adjusted for age, maximized the sensitivity and speci?city for the diagnosis of organic disease,correctly discriminating the cause of diarrhea in82%of the study population,with a positive predictive value of80.4%and a negative predictive value of 77.7%.The power of the model did not change our reclas-sifying diverticulosis as functional condition or excluding small polyps(?1cm)from the analysis,as suggested by common clinical sense.Finally,knowing the high sensitiv-ity of the L/M test for celiac disease,we tried our model without this group of patients.The positive predictive value was70.5%and the negative predictive value77.2%,indi-cating that the good performance of our model was not strongly biased by the high number of celiac disease patients in our population.
Although at the univariate statistic low serum iron level was signi?cantly associated with the presence of organic disease,it was not a signi?cant predictor at the multivariate level.A possible explanation for this discrepancy is that this test has a performance comparable to the L/M test.In particular,iron de?cient anemia can be the only presenting sign of small bowel disease(38).On the other hand,CRP, being a more sensitive parameter for detecting in?ammation (39),offered signi?cant additional discriminating informa-tion to our model.
As a matter of fact,our model was not able to sort almost20%of the patients presenting with chronic diar-rhea.The most common organic causes of chronic diar-rhea in our population and in similar ones(22,30)were malabsorption and in?ammation.Indeed the actual value of the combination of L/M test and CRP were in their ability to screen for these two conditions.However, among organic causes of chronic diarrhea,conditions are included in which the symptoms are caused by different mechanisms,such as altered motility or malignancy.For example,in a conspicuous number of patients we found diverticula to be associated with chronic diarrhea.In the majority of these patients,intestinal permeability was in the range of normal.This is not surprising,inasmuch as diarrhea in diverticular disease is mainly caused by co-existent motility problems or dysmicrobism(40),which do not have a direct effect on epithelial permeability(6). Furthermore the mean age of patients with diverticula was signi?cantly higher(59?14yr)compared to that in the rest of the population.Because the probability of ?nding an organic disease in patients aged?50yr who present with chronic diarrhea is statistically increased,we think that a more invasive diagnostic approach after the ?rst observation is justi?ed in these circumstances.
In our series of patients,approximately50%have been diagnosed with a functional condition,in agreement with previous reports(30,41).A total of120patients had a ?nal diagnosis of IBS that was con?rmed during the follow-up,with L/M test being altered in?ve cases.In all, 76upper GI endoscopies,68colonoscopies,and13ra-diological procedures were performed,with46patients undergoing both endoscopic procedures to reach a diag-nosis.Even if the IBS diagnosis frequently remains an exclusion diagnosis,the?nding of a normal intestinal permeability test could help in avoiding an aggressive workup,at least in young patients.The signi?cance of normal intestinal permeability in characterizing IBS pa-tients is endorsed by a recent study(42).
In the group with functional disorders we included17 patients for whom the only?nding was ileal follicular hy-perplasia in the absence of alteration of serum gamma globulin.Such an endoscopic and histological picture is quite common,especially in young patients,although it may represents a predisease condition(43)or even a preneoplas-tic status(44).We found increased intestinal permeability in seven of our patients with follicular hyperplasia.During the follow-up,10patients,including the seven with altered L/M test,underwent ileal biopsies and L/M tests for a second time.Eight of them had recovered both clinically and his-tologically during the follow-up;one has been diagnosed with Crohn’s disease;and one still had follicular hyperplasia after36months.Only in the latter two patients were the LM test results con?rmed to still be altered.
In conclusion,a test of permeability to sugars remarkably increases the diagnostic ability of?rst-line biochemical tests.In combination with CRP this test is able to discrim-inate more than80%of patients presenting with chronic diarrhea of unknown origin.Furthermore,the L/M test is also con?rmed to be strongly predictive of small bowel disease.We propose to include the L/M test in the?rst-level evaluation in patients with chronic diarrhea because of its substantial helpfulness in the diagnostic evaluation and in avoiding unnecessary and aggressive workup. ACKNOWLEDGMENTS
This work was accomplished in the Gastroenterology Sec-tion,Department of Surgical and Gastroenterological Sci-ences,University of Padova,Padova,Italy.
2250Di Leo et al.AJG–Vol.98,No.10,2003
Reprint requests and correspondence:Giacomo C.Sturniolo, M.D.,Department of Surgical and Gastroenterological Science, Gastroenterology Section,c/o Ospedale Civile,Via Giustiniani2 35128Padova,Italy.
Received Jan.9,2003;accepted May19,2003. REFERENCES
1.Read NW,Krejs GJ,Read MG,et al.Chronic diarrhea of
unknown origin.Gastroenterology1980;78:264–71.
2.Talley NJ,Weaver AL,Zinsmeister AR,et al.Onset and
disappearance of gastrointestinal symptoms and functional gastrointestinal disorders.Am J Epidemiol1992;136:165–77.
3.Fine KD,Seidel RH,Do K.The prevalence,anatomical dis-
tribution and diagnosis of colonic causes of chronic diarrhea.
Gastrointest Endosc2000;51:318–26.
4.Afzalpurkar RG,Schiller LR,Little KH,et al.The self-limited
nature of chronic idiopathic diarrhea.N Engl J Med1992;327: 1849–52.
5.Hollander D.Intestinal permeability,leaky gut,and intestinal
disorders.Curr Gastroenterol Rep1999;1:410–6.
6.Bjarnason I,MacPherson A,Hollander D.Intestinal perme-
ability.An overview.Gastroenterology1995;108:1566–81.
7.Bjarnason I,Maxton D,Reynolds AP,et al.A comparison of
4markers of intestinal permeability in control subjects and patients with coeliac disease.Scand J Gastroenterol1994;26: 630–9.
8.Jenkins RT,Jones DB,Goodacre RL,et al.Reversibility of
increased intestinal permeability to51-Cr EDTA in patients with gastrointestinal in?ammatory diseases.Am J Gastroen-terol1987;82:1159–64.
9.Zhang Y,Lee B,Thompson M,et al,and the Diarrhea Work-
ing Group,https://www.wendangku.net/doc/ea12592590.html,ctulose-mannitol intestinal permeability test in children with diarrhea caused by rotavirus and crypto-sporidium.J Pediatr Gastroenterol Nutr2000;31:16–21. 10.Alam AN,Sarker SA,Wahed MA,et al.Enteric protein loss
and intestinal permeability changes in children during acute shigellosis and after recovery:Effect of zinc supplementation.
Gut1994;35:1707–1.
11.Zuckerman MJ,Watts MT,Bhatt BD,et al.Intestinal perme-
ability to21Cr-EDTA in infectious diarrhea.Dig Dis Sci 1993;38:1651–7.
12.Schrander JJP,Unsalan-hooyen RWM,Forrest PP,et al.
51CrEDTA intestinal permeability in children with cow’s milk intolerance.J Pedriatr Gastroenterol Nutr1990;10:189–92.
https://www.wendangku.net/doc/ea12592590.html,abam SO,Mann RJ,Cooper BT.Small intestinal perme-
ability to sugars in patients with atopic eczema.Br J Dermatol 1984;110:649–52.
14.Juby LD,Rothwell J,Axon https://www.wendangku.net/doc/ea12592590.html,ctulose/mannitol test:An
ideal screen for coeliac disease.Gastroenterology1989;96: 79–85.
15.Vogelsang H,Genser D,Wyatt J,et al.Screening for coeliac
disease:A prospective study on the value of non invasive tests.
Am J Gastroenterol1995;90:394–8.
16.Hamilton I,Cobden I,Rothwell J,et al.Intestinal permeability
in coeliac disease:The response to treatment and single-dose gluten challenge.Gut1982;23:202–10.
17.Wyatt J,Vogeslang H,Hubl W,et al.Intestinal permeability
and the prediction of relapse in Crohn’s https://www.wendangku.net/doc/ea12592590.html,ncet1993;
34:1437–9.
18.D’Inca`R,Di Leo V,Corrao G,et al.Intestinal permeability
test as a predictor of clinical course in Crohn’s disease.Am J Gastroenterol1999;94:2956–60.
19.Corcoran A,Page I.A method for determination of mannitol
in plasma urine.J Biol Chem1947;170:165–71.
20.Behrens RH,Docherty H,Elia M,et al.A simple enzymatic
method for the assay of urinary lactulose.Clin Chim Acta 1984;137:361–67.
21.Hosmer DW,Lemeshow S.Applied logistic regression.Sec-
ond ed.Toronto:John Wiley&Sons,2000.
22.Fine K,Schiller LR.AGA technical review on the evaluation
and management of chronic diarrhea.Gastroenterology1999;
116:1464–86.
23.Uil JJ,van Elburg RM,van Overbeek FM,et al.Clinical
implications of the sugar absorption test:Intestinal permeabil-ity test to asses mucosal barrier function.Scand J Gastroen-terol1997;223(suppl1):70–8.
24.Ford RPK,Menzies IS,Phillips AD,et al.Intestinal sugar
permeability:Relationship to diarrhoeal disease and small bowel morphology.J Pediatr Gastroenterol Nutr1985;4:568–
74.
25.D’Inca`R,Di Leo V,Martines D,et al.Permeability to sugars
can be helpful in predicting disease activity in Crohn’s disease.
Gastroenterology1992;102:A616.
26.Keshavarzian A,Fields JZ,Vaeth J,et al.The differing effects
of acute and chronic alcohol on gastric and intestinal perme-ability.Am J Gastroenterol1994;89:2205–11.
27.Andre F,Andre C,Feknous M,et al.Digestive permeability to
different-sized molecules and to sodium cromoglycate in food allergy.Allergy Proc1991;12:293–98.
28.Fine KD,Ogunji F,George J,et al.Utility of a rapid fecal latex
agglutination test detecting the neutrophil protein,lactoferrin, for diagnosing in?ammatory causes of chronic diarrhea.Am J Gastroenterol1998;93:1300–5.
29.Limburg PJ,Ahlquist DA,Sandborn WJ,et al.Fecal calci-
protein level predict colorectal in?ammation among patients with chronic diarrhea referred for colonoscopy.Am J Gastro-enterol2000;95:2831–7.
30.Bytzer P,Stokholm M,Andersen I,et al.Aetiology,medical
history and fecal weight in adult patients referred for diarrhea:
A prospective study.Scand J Gastroenterol1990;25:572–8.
31.Schiller LR.Diarrhea.Med Clin North Am2000;5:1259–72.
32.Juby LD,Rothwell J,Axon ATR.Cellobiose-mannitol test–a
sensitive tubeless test for coeliac disease:Results on1010 unselected patients.Gut1989;30:476–80.
33.Smecuol E,Bai JC,Vasquez H,et al.Gastrointestinal perme-
ability in coeliac disease.Gastroenterology1997;112:1129–
36.
34.Catassi C,Fabiani E,Ratsch IM,et al.Is the sugar intestinal
permeability test a reliable investigation for coeliac disease screening.Gut1997;40:215–7.
35.Uil JJ,Van Elburg RM,Janssens PM,et al.Sensitivity of a
hyperosmolar or“low”-osmolar test solution for sugar absorp-tion in recognizing small intestinal mucosal damage in coeliac disease.Dig Liver Dis2000;32:195–200.
36.Shamir R,Lerner A,Shinar E,et al.The use of a single
serological marker understimates the prevalence of celiac dis-ease in Israel:A study of bloody donors.Am J Gatroenterol 2002;97:2589–94.
37.Fasano A,Berti I,Gerarduzzi T,et al.Prevalence of celiac
disease in at-risk and not-at-risk groups in the United States.A large multicentric study.Arch Intern Med2003;163:286–92.
38.Ackerman Z,Eliakim R,Stalnikowicz R,et al.Role of small
bowel biopsy in the endoscopic evaluation of adults with iron de?ciency anemia.Am J Gastroenterol1996;91:2099–102.
39.Schultz DR,Arnold PI.Properties of four acute phase pro-
teins:C-reactive protein,serum amyloid A protein,alpha 1-acid glycoprotein,and?brinogen.Semin Arthritis Rheum 1990;20:129–47.
40.Young-Fadok TM,Roberts PL,Spencer MP,et al.Colonic
diverticular disease.Curr Probl Surg2000;37:457–514. 41.Bertomeu A,Ros E,Barragan V,et al.Chronic diarrhea with
2251
AJG–October,2003Lactulose/Mannitol Test in Chronic Diarrhea
normal stool and colonic examinations:Organic or functional.
J Clin Gastroenterol1991;13:531–6.
42.Tibble JA,Sightorsson G,Foster R,et https://www.wendangku.net/doc/ea12592590.html,e of surrogate
markers of in?ammation and Rome criteria to distinguish organic from nonorganic intestinal disease.Gastroenterology 2002;123:450–60.43.Molas G,Potet F,Nogig P.Focal lymphoid hyperplasia
(pseudolymphoma)of the terminal ileum in adults.Gastroen-terol Clin Biol1985;9:630–3.
44.Bastlein C,Burle?nger R,Holzberg E,et https://www.wendangku.net/doc/ea12592590.html,mon variable
immunode?ciency syndrome and nodular lymphoid hyperpla-sia in the small intestine.Endoscopy1988;20:272–5.
2252Di Leo et al.AJG–Vol.98,No.10,2003
